012 年欧洲泌尿协会睾丸癌指南(转载)
Testicular cancer represents between 1% and 1.5% of male neoplasms and 5% of urological tumours in general, with 3-10 new cases occurring per 100,000 males/per year in Western society. An increase in the incidence of testicular cancer was detected during the 1970s and 1980s, particularly in Northern European countries, and there is a clear trend towards an increased testicular cancer incidence in the last 30 years in the majority of the industrialised countries in North America, Europe and Oceania, although surprising differences in incidence rates are seen between neighbouring countries (4,5). Data from the Surveillance Epidemiology and End Results Program during the years 1973 to 1998 show a continuing increased risk among Caucasian men in the USA only for seminoma.郑州大学三附院泌尿外科郭丙涛
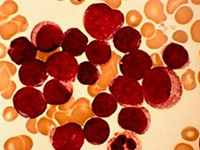
Only 1-2% of cases are bilateral at diagnosis. The histological type varies, although there is a clear predominance (90-95%) of germ cell tumours . Peak incidence is in the third decade of life for nonseminoma, and in the fourth decade for pure seminoma. Familial clustering has been observed, particularly among siblings.
Genetic changes have been described in patients with testicular cancer. A specific genetic marker (an isochromosome of the short arm of chromosome 12 C i(12p) C has been described in all histological types of germ cell tumours. Intratubular germ cell neoplasia (testicular intraepithelial neoplasia, Tin) shows the same chromosomal changes, and alterations in the p53 locus have been found in 66% of cases of testicular Tin.
A deregulation in the pluripotent programme of fetal germ cells (identified by specific markers such as M2A, C-KIT and OCT4/NANOG) is probably responsible for the development of Tin and germ cell neoplasia. There is overlap in the development to seminoma and embryonal carcinoma as shown by genomewide expression analysis and detection of alpha-fetoprotein (AFP) mRNA in some atypical seminoma. Continued genome wide screening studies and gene expression analysis data suggest testis cancer specific gene mutations on chromosomes 4, 5, 6 and 12 (namely expressing SPRY4, kit-Ligand and Synaptopodin).
Epidemiological risk factors for the development of testicular tumours are: a history of cryptorchidism or undescended testis (testicular dysgenesis syndrome), Klinefelter’s syndrome, familial history of testicular tumours among first-grade relatives (father/brothers), the presence of a contralateral tumour or Tin, and infertility (14-20). Tallness was associated with a risk of germ cell cancer, although further confirmation is needed.
Testicular tumours show excellent cure rates. The main factors contributing to this are: careful staging at the time of diagnosis; adequate early treatment based on chemotherapeutic combinations, with or without radiotherapy and surgery; and very strict follow-up and salvage therapies. In the past decades, a decrease in the mean time delay to diagnosis and treatment has been observed. In the treatment of testicular cancer, the choice of centre where this treatment is going to be administered is of utmost importance. Although early stages can be successfully treated in a non-reference centre, the relapse rate is higher. In poor prognosis non-seminomatous germ cell tumours, it has been shown that overall survival within a clinical trial depended on the number of patients treated at the participating centre (worse < 5 patients enrolled). In the same context, the frequency of post-chemotherapy residual tumour resection is associated with perioperative mortality and overall survival.
- 上一篇:睾丸癌是传染性的疾病吗
- 下一篇:活着:一个睾丸癌患者的心声
- 本文延伸阅读
相关文章
- 睾丸癌是传染性的疾病吗
- 睾丸癌会不会传染
- 睾丸癌能传染给别人吗
- 得了睾丸癌会传染吗
- 睾丸癌会发生传染吗
- 睾丸癌会传染吗
- 睾丸癌究竟会不会传染呢
- 睾丸癌是不是传染病呢
- 睾丸癌科普
- 睾丸癌临床进展
- 睾丸癌会不会传染呢
- 提高家长对隐睾症疾病的认识
免费提问